March is Women’s History month and hosts International Women’s Day. It’s also Endometriosis awareness month, a disease that affects an estimated 200 million women worldwide, which translates to roughly 10% of reproductive age women and girls.1
Endometriosis is a disease where tissue similar to the lining of the uterus grows outside the uterus, causing pain and/or infertility. It can take years to diagnose, which is unfortunately an all-too-common reality for many. The longer it goes undiagnosed, managed or treated, the worse the condition can become. Raising awareness and understanding of this disease is essential in order to encourage more women to seek medical help for this drastically under-diagnosed condition.
We spoke to a Shields’s patient, Tracy (the name of our patient has been changed to maintain confidentiality and respect their privacy), about her experience with undiagnosed endometriosis and the impact it had on her life. It took four years for Tracy to be diagnosed with Endometriosis. Her pain was chronic, severe, and worsened to excruciating during her periods.
Tracy first noticed something when her daughter was about a year old, a short time after she stopped breastfeeding. She told her gynecologist: “Something is really wrong. I am having labor and delivery flashbacks when I get my period. This can’t be normal.”
Her doctor’s first instinct was to get a transvaginal ultrasound, where she thought she spotted an ovarian cyst. This was monitored with regular ultrasounds with inconsistent results that puzzled her doctor. As Tracy unfortunately found out, endometriosis can often present symptoms that look like other conditions and contribute to a diagnostic delay.2 In her case, diagnosis took four years. Four years marked by seven inconclusive ultrasounds, two biopsies, worsening pain, and ever-lengthening menstrual periods.
Tracy feels the diagnosis could have been identified much sooner with an MRI scan, in addition to pelvic ultrasound. MRI is excellent at detecting smaller sites of endometriosis, especially along the bowel and pelvic ligaments. Deeper structures are difficult to see by ultrasound and an MRI exam is often necessary for an accurate diagnosis. Further, a proper diagnosis at an early stage can prevent the progression of the disease, potentially lessening the impact of surgery, recovery and, most importantly, pain management. To demonstrate the vast underuse of MRI for endometriosis, this MRI scan type made up less than 1% of the total MRI scans done in 2021 across the Shields network. For a disease affecting about 10% of women, that statistic is shockingly low.
Even after suggesting an MRI to her provider several times, Tracy was told that the ultrasound technology was the best solution. Why? Ultrasound is a common and comfortable technology for gynecology that is used often. It’s typically located right in the doctor’s office which makes it easily accessible and readily available. While ultrasound is an excellent diagnostic tool for many gynecological conditions, MRI is widely acknowledged as the best option for diagnosis of endometriosis. Despite advocating for an MRI, Tracy continued at the advisement of her gynecologist and underwent an endometrial ablation. This is an outpatient procedure that removes a thin layer of tissue (endometrium) from the uterus. It is done to stop or reduce heavy menstrual bleeding, but is only an option for women who do not plan to have any children in the future.3
But the pain just got worse.
“When you have this ablation, and you have endometriosis and don’t know it … it lit a fire inside my body. My pain accelerated exponentially from the moment I had the procedure until my next period.”
Tracy was at the end of her rope. The gynecologist wanted to go in laparoscopically and remove the cyst, the ovary, and the fallopian tube. Tracy Did not want to do that until she got an MRI, so they could know what to expect, and was prepared to seek a second opinion. Her doctor finally agreed to order an MRI.
The results were “a mess”. The radiologist said she was “loaded with Endometriosis gone wild”, with endometrium growing into her intestines. Tracy's Resulting surgery was still completed laparoscopically, but took seven hours and three physicians: her gynecologist, a gastrointestinal specialist, and a surgeon familiar with complex endometriosis cases.
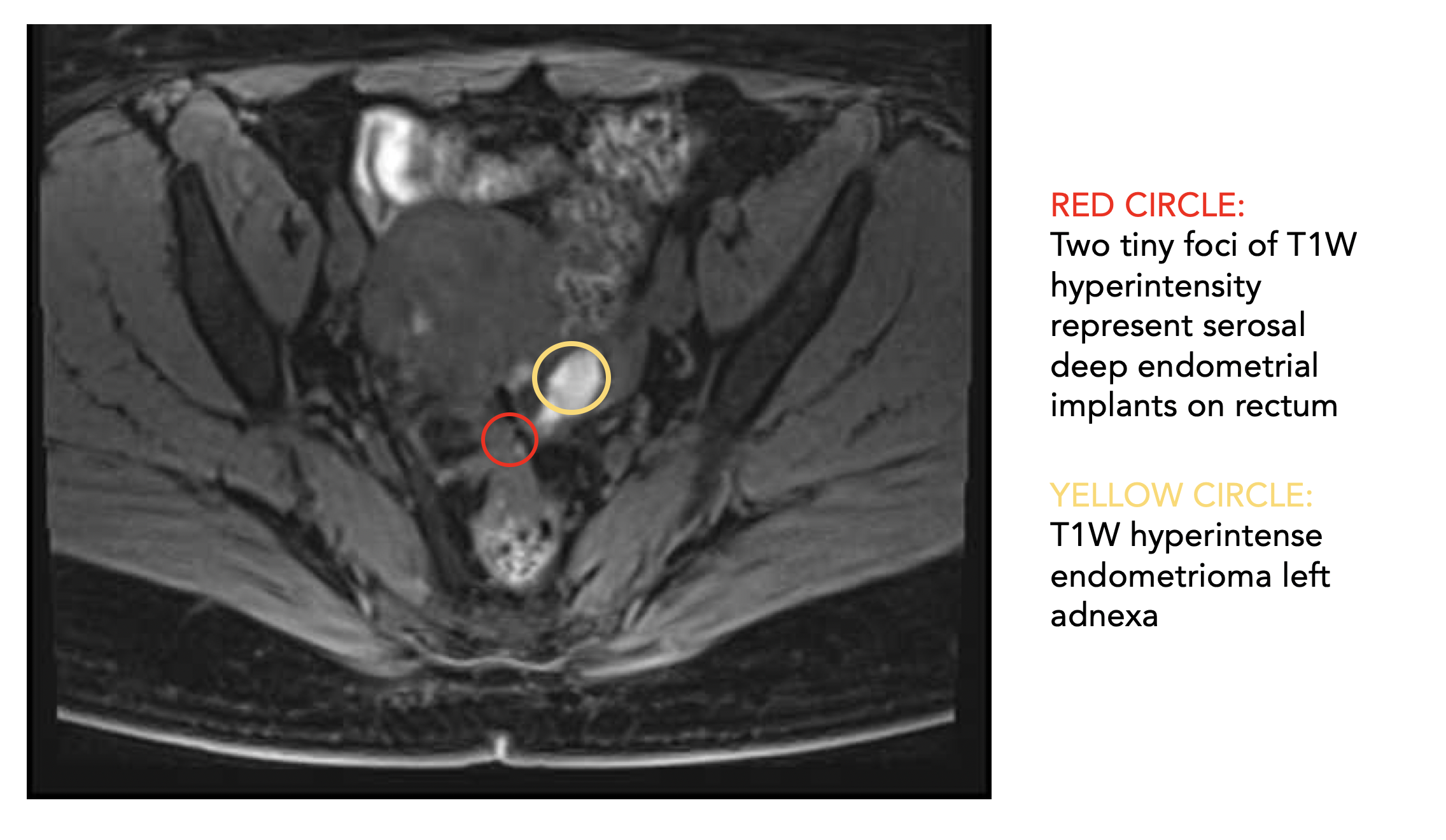
In Tracy’s case, ultrasound was able to pick up the lesion on the ovary, but none of the endometriosis on the rectum. The implants (pictured here in the MRI scan) could only be seen by MRI as ultrasound is limited in scope and can only see the ovary.
“It just never should have gotten to that point”, Tracy laments. She was frustrated and angry. All those years of pain – and the financial burden. Tracy says she lost track of what the bills got to before she reached her deductible every year. “So unnecessary. If I had an MRI right away, we would have had this diagnosis four years earlier. Not only would my surgery not have been a seven hour ordeal - maybe I would not even have needed a complete hysterectomy. What about younger women who are only in their thirties, and still want to have children? I kept thinking about that. How lucky I was that it didn’t affect me until this stage of my life.”
Treatment for Endometriosis doesn't always have to involve surgery, it depends on the effectiveness in the individual, side effects, long-term safety, availability, and costs. Most current hormonal management is not suitable for those who wish to get pregnant, since they affect ovulation. Surgery can remove endometriosis lesions, adhesions, and scar tissue, but success in alleviating symptoms depends on the extent of the disease. Tracy’s case was advanced, but luckily the surgery was successful.
Too often, the women are not aware that pelvic pain is not ‘normal’, leading to a normalization and stigmatization of symptoms and significant diagnostic delay.4 Greater informational campaigns are needed to educate healthcare providers and women the world over about normal and abnormal menstrual health and systems. This should include ensuring that screening and identifying Endometriosis is possible with enhancing the availability of magnetic resonance imaging.
Education should include a full list of symptoms and possible causes to fully equip women to advocate for themselves against a disease which can cause severe pain, fatigue, depression, and infertility.
The best tool for diagnosis is careful history of menstrual symptoms – noting any and all pain associated with menstruation. Enhanced awareness, early diagnosis, and management can reduce the long-term burden of its systems – a worthy goal.
As a start:
Symptoms associated with endometriosis vary, and include a combination of:5
- painful periods
- chronic pelvic pain
- pain during and/or after sexual intercourse
- painful bowel movements
- painful urination
- fatigue
- depression or anxiety
- abdominal bloating and nausea
For more information there are articles on the World Health Organization website, The U.S. Department of Health and Human services’ Office on Women’s Health, and the Mayo Clinic. Always talk to your doctor about any menstrual pain you are experiencing, and see if an MRI is appropriate for your case.
Shields offers pelvic MRI scans for diagnosis of endometriosis at every MRI center across our network as well as subspecialty expertise in this type of scan. Our radiologists work closely with your physician to get your results quickly to get you on the path to recovery. Shields is committed to creating the best experience possible, providing our patients with comfort and the best quality care. Check out our website to find the location closest to you, and to learn more about our commitment to patient service.
https://shields.com/find-location/
Additional Resources:
Endometriosis Association - Phone Number: 414-355-2200
Endometriosis Foundation of America - Phone Number: 646-854-3337
Endometriosis Research Center - Phone Number: 800-239-7280



